A big few months as we hurtle towards the end of the year. It has been an incredibly news-heavy number of weeks; with funding extensions, the Federal budget, updates to the Government’s funding reform project, Royal Commission hearings and special reports, and everything in between.
As always, we acknowledge that resources, information and support are of the most importance currently and with so much in the news, that a breakdown of what we need to know is a priority. In this COVID update we will lay out the budget and COVID funding figures, recent updates and government announcements, along with resources and guides available to our community especially during this period.
There are many excellent resources out there, and we highly recommend keeping up to date with all the Aged Care peak bodies, who continue to provide a great deal of support and information in this time; the Ageing Agenda, Talking Aged Care, the Weekly Source & the Donaldson Sisters for timely Aged Care news; and the Department of Health updates.
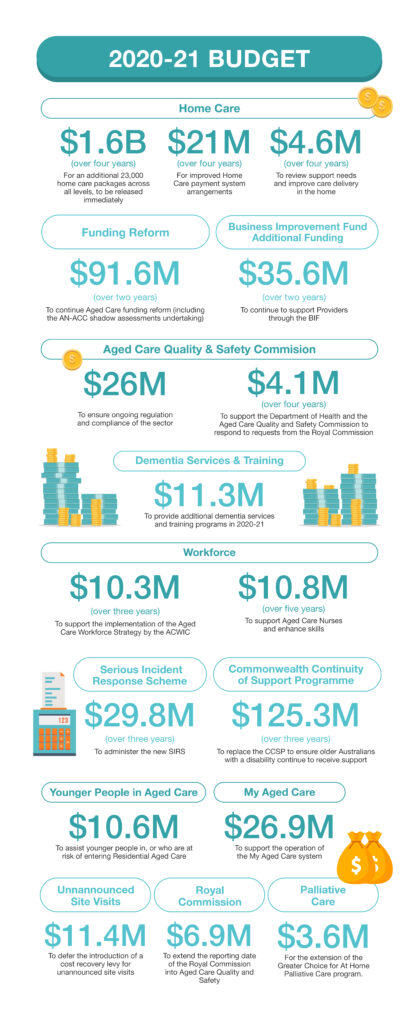
2020-21 BUDGET
The delayed 2020 budget was announced in October, with a focus on Home Care, but little relief for Residential Providers. The budget saw $1.6B for 23,000 new Home Care packages across all levels, which will be released immediately. A further $4.6M over two years from 2020-21 is set to review care and establish how care and support in the home can be best delivered. $91.6M will be allocated over the next 2 years for Aged Care funding reform, including the undertaking of the AN-ACC ‘Shadow Assessment’ (you can read further information on this below). For a breakdown of the Aged Care budget, you can view the Aged Care Budget Fact sheets, the Weekly Source’s wrap up, or our 2020-21 Budget breakdown below.
With the Royal Commission’s Final report due in February 2021, it is expected that the 2021-22 budget will see a focus on Aged Care; Minister Richard Colbeck referencing the need for the May 2021 budget to resource the Commission’s recommendations in his LASA Congress address; and treasurer Josh Frydenberg noting that more funding will be allocated post the Final Report.
While the addition of 23,000 new Home Care Packages has been welcomed, disappointment has been expressed over the lack of funding for Residential Care. Peak bodies Aged & Community Services (ACSA) and Leading Age Services Australia (LASA) shared their thoughts following the budget, with ACSA CEO Pat Sparrow welcoming the Home Care packages, but noting that thousands of people would still be waiting for ‘the right level of support or any support at all’. Furthermore she highlighted that the budget included ‘small but useful initiatives’, but the Aged Care system needs a reboot and a total rethink, as opposed to propping up the current system. LASA reflected similar sentiments in that the budget announcements are a start, but more investment is required. Prior to the Budget announcements, COTA Australia released the Safer at Home campaign, calling for funding for and additional 60,000 Home Care packages, and a wait period of no longer than 30 days. Although pleased to see 23,000 packages announced, COTA CEO Ian Yates was disappointed that there was no commitment to reducing the waiting times and stated that there is still a long way to go. StewartBrown’s Budget analysis on its impacts on the Aged Care sector has highlighted the package level distribution, with Level 4 packages allocated the least amount (2,000), in comparison to Levels 1 (5,000), 2 (8,000) and 3 (8,000).
Prior to the budget release the independent public policy think tank, Grattan Institute, communicated three key areas the Government should focus the budget allocation on in Aged Care: Home Care, greater transparency in the sector, and a rescue package for Residential Care.
ROYAL COMMISSION: SPECIAL COVID-19 REPORT & FINAL HEARING
As always, another busy period for the Royal Commission. October saw the final hearing in the Royal Commission into Aged Care Quality and Safety. On the 22 and 23 of October, the Counsel Assisting’s Final Submissions were heard, submitting 124 Recommendations for consideration. You can read Counsel Assisting’s Final Submissions and Proposed Recommendations here. Interested parties are able to respond to the final submissions by written submission. The due date for these responding submissions is 12 November 2020.
The longest hearing seen by the Royal Commission was the inquiry into Funding, financing and prudential regulation, held from 14 – 22 September.
In September, the Commission released Capital Financing For Residential Aged Care: Call For Submissions, a paper defining the history of capital financing arrangements and how they currently operate in Residential Aged Care, with a call for submissions that were due in early October. Concurrently, an additional publication was released titled The Required Return For Aged Care Service Providers, a paper by an economics consultancy firm Frontier Economics which develops a ‘building block’ model ‘to determine an appropriate allowance for the return on capital and return of capital (depreciation) for providers of aged care accommodation services.’
Two further Research Papers by the National Ageing Research Institute (NARI) followed in October. Research Paper 14, Inside The System: Home And Respite Care Clients’ Perspectives and Research Paper 15, Inside The System: Aged Care Residents’ Perspectives, share the findings of surveys undertaken by NARI on how people living in Residential Aged Care or receiving care in the home, feel about their care and the concerns they had.
After the hearing inquiring into the COVID-19 pandemic impact and the response of Aged Care, the Commissioner’s special report was handed down on 1 October. The report identified ‘four areas for immediate action’ and six recommendations, all of which the Government accepted. The recommendations are as follows:
The six recommendations from the special report are:
- Recommendation 1 – Implementation
- Recommendation 2 – Visitors and quality of life
- Recommendation 3 – Allied health
- Recommendation 4 – An aged care plan and advisory body
- Recommendation 5 – Infection control expertise and personal protective equipment
- Recommendation 6 – Infection control training
(You can read a breakdown of each recommendation here.)
Recommendation 1 requires the government to report on the implementation of the report’s recommendations by 1 December 2020. While the report states that it is not the time for blame, it concludes that the Government’s preparedness for the crisis was insufficient, with a lack of leadership and inconsistent messaging. In September, Minster Colbeck was censured by the Senate for neglecting to take responsibility for the COVID-19 outbreaks across Aged Care.
Separately to the Royal Commission, the Grattan Institute released a report focusing on the need for an overhaul of the system, more funding and personalised care plans. You can read the report, ‘Rethinking aged care: emphasising the rights of older Australians’ report‘ here.
You can read the Commissioner’s Aged Care and COVID-19: A Special Report here and the official Government response to the report from Aged Care Minister Richard Colbeck here.
With a great deal of media reports surrounding the Royal Commission, the Aged Care Guide, Australian Ageing Agenda and The Weekly Source are excellent sources of information. You can also access live and past hearings via the Royal Commission webcast channel here.
FUNDING & FINANCE
As always, funding the Aged Care sector has been at the forefront of news for the industry, and even more so recently with the Royal Commission’s funding and finance hearings and the release of the 2020-2021 budget. The funding hearings were the longest seen at the Royal Commission, running over 7 days, and they heard a number of future funding ideas and opinions for the sector. These included HECs style loans, four streams with different funding models, wariness around additional taxes and levies and care recipients contributing more to their costs if they could. The conversation on funding models and financing the sector continued post the hearings, with Natasha Chadwick, CEO of NewDirection Care sharing 7 different points for funding changes; CEO of Catholic Healthcare Australia, Pat Garcia suggesting superannuation style Health Savings accounts; and Darrell Price, who is the principal and national head of health and aged care at Grant Thornton, also suggesting measures embedded in superannuation and user-pay approaches. The Government was also criticised by Counsel Assisting for the 2013-14 and 2016-17 ACFI indexation freezes.
For the full detail of the Hearing, we recommend viewing the Hearing transcripts or the audio via the Royal Commission webcast channel here.
The Royal Commission’s Research Paper 11 – Aged care reform: projecting future impacts prepared by Deloitte Access Economics, reported that a 1.01% tax increase, or 0.89% Medicare levy increase would fund the Aged Care system for ‘4-star’ staffing level care (based on the US staffing model). A 1% increase falls below the 3.1% increase in tax that 10,000 participants surveyed for Research Paper 6 said they would be willing to pay. Prime Minister Scott Morrison stated that a Medicare Levy hike was not in the Government’s plan. Earlier in September, Health Services Union’s (HSU) final submission to the Royal Commission, a report titled Delivering Decent Residential Aged Care (written in partnership with consultancy firm Equity Economics) called for a Medicare levy hike to better fund Aged Care.
Aged Care funding was also heavily reported in the media following the release of Research Paper 12 – Report on the profitability and viability of the Australian aged care industry. The report found that 74% of Aged Care Providers were making a profit, with only 13% making a loss, a stark contrast to recent StewartBrown financial performance survey findings. The report findings were challenged by Grant Corderoy of StewartBrown, noting that the financial information provided to BDO, the company commissioned to do the report, was incomplete and did not show the full story. The report authors also noted that financial performance and transparency of the data was unclear, due to a number of factors, including limited reporting obligations.
StewartBrown’s Aged Care Financial Performance Survey for the year to 30 June 2020 has been released, reporting that 64% of Providers now operating at a loss. The figure follows the trend of previous reports, with the number of Providers operating at a loss increasing. The StewartBrown report Listed Aged Care Providers Financial Performance Analysis released in early October also showed a slow in growth for listed Providers.
MINISTER FORESHADOWS LEGISLATION REWRITE RECOMMENDATION
At the 2020 LASA National Congress (held as a virtual event this year), Aged Care Minister Richard Colbeck addressed delegates for 18 minutes. The Minister flagged the importance of the Royal Commission and actioning its recommendations when the final report is released in February 2021, as well as highlighting the hard work undertaken by the Aged Care industry. However, the Minister also highlighted that the challenging work would continue post-COVID with ‘a lot to be done’ post the Royal Commission’s final report. This, he noted, included the possibility of rewriting the Aged Care Act, which came prior to the release of the Royal Commission’s Counsel Assisting recommending the rewrite. With the Royal Commission’s ‘forensic view’ into the industry and its recommendations, Minister Colbeck noted that part of the process of responding to the Final Report, could mean a rewrite of the Aged Care Act, which became apparent on the release of the recommendations on the 22 October 2020.
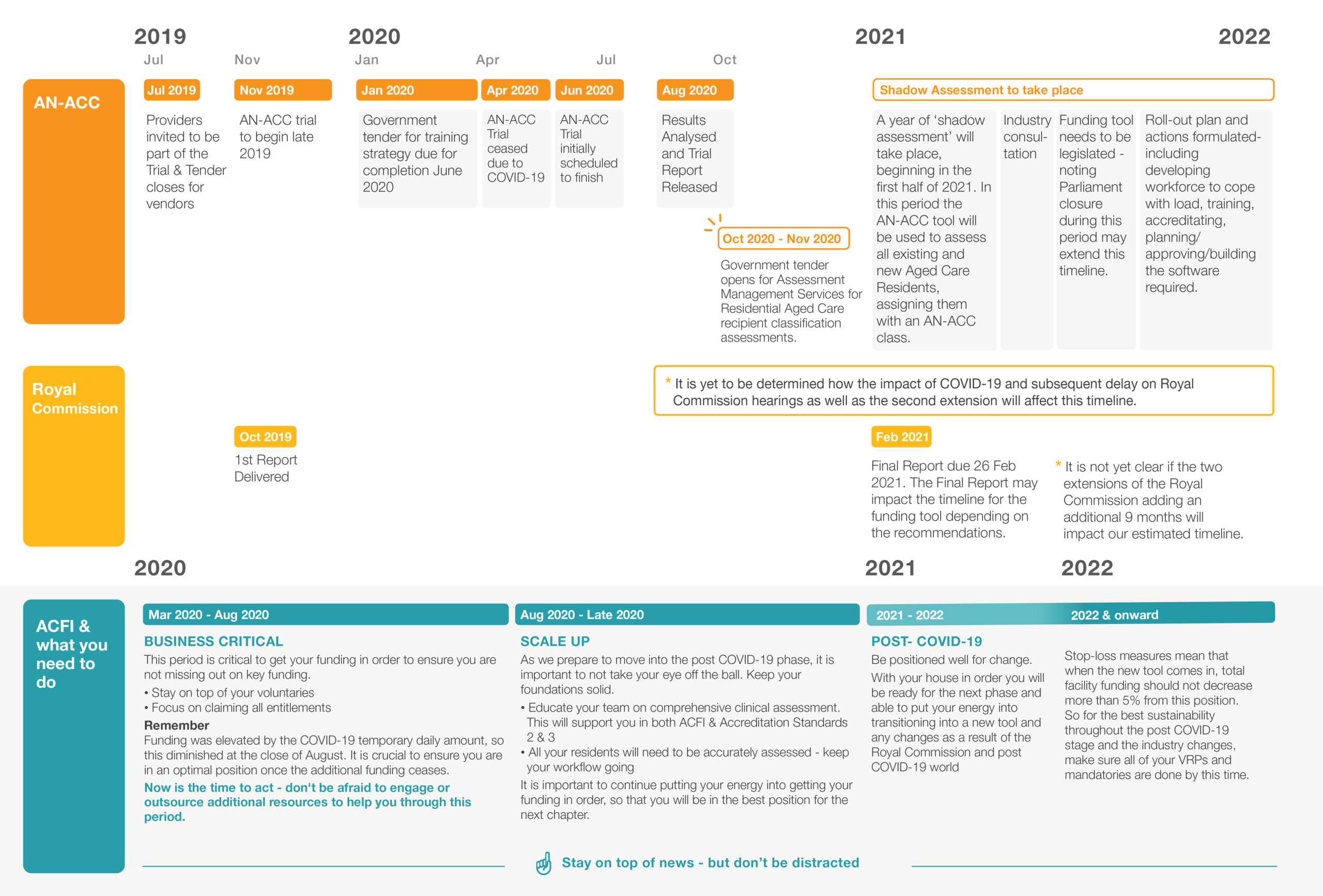
AN-ACC UPDATES
This October the Government announced updates on the funding reform trial for the proposed Australian National Aged Care Classification (AN-ACC) model. The AN-ACC assessment trial, that had been underway since late 2019 and scheduled to be completed in June 2020 was put on hold in March 2020 as a result of the COVID-19 outbreak. Originally slated to be on hold for at least 6 months, the trial was ceased from early April 2020 and the trial report released on the data that had been collected up to this point, which was made up of:
- 7387 AN-ACC assessments completed of which:
- 7276 permanent residents
- 111 respite residents
- Across 122 homes
The trial was originally aiming to involve the assessment of up to 12,000 Residents. You can read the Report on the AN-ACC trial here.
The next step in the funding reform project will be a ‘Shadow Assessment’ period. This will involve a year of the AN-ACC tool being used to assess and an AN-ACC class assigned to all existing and new Aged Care Residents. The shadow assessment is expected to begin in early 2021, and will run alongside the current ACFI funding tool, with all funding still via ACFI. A call for tenders for independent assessors to conduct the assessments closes on the 13th November, with the proposed assessment period running from March 2021 to February 2022 (and a possible extension to June 2022 if deemed necessary). The tender documentation states that the Australian government is committed to executing the Assessment and Classification model components of the AN-ACC model, but has made no decision on the funding element.
While there has been some movement occurring in this space, it is important to note that the Government has not decided to implement the proposed funding model and will continue to undertake investigation into potential models and consult with the industry. For a breakdown on the changes that a new tool, the Royal Commission and the post-COVID world will bring, view our estimated timeline below.
PRODA & THE NEW AGED CARE PROVIDER PORTAL FOR ONLINE CLAIMING
Many Aged Care Providers will be aware that Services Australia (Medicare) are in the process of moving to PRODA as part of their digital roadmap. We’ve written an article series with the most important details to help Providers transition to Service Australia’s new digital identity verification system (PRODA) and the new online claiming portal (Aged Care Provider Portal). Start the series with our Frequently Asked Questions here, or you can refer to Services Australia’s information on PRODA here, and information on the Aged Care Provider Portal (ACPP) here. The cut off for the use of the Aged Care Online Claiming (ACOC) Portal is the 20th November 2020, so the time to back up your data and transition to using PRODA and the ACPP, is now!
Not sure where to start?
ADDITIONAL FUNDING FOR COVID-19 RELATED COSTS
There have been multiple announcements this year for additional funding for the Aged Care sector to assist with COVID-19 related costs, through both supplements being paid to Providers and grants made available. In addition to the recently released budget figures for Aged Care, there are a number of announcements to keep up with, so we’ve broken down what has been announced.
In March, the Government announced $444.6M in additional funding to support the industry amidst the pressures of tackling COVID-19. For an overview of the inclusions, please refer to Minister Richard Colbeck’s media release here.
As a part of this funding:
- $78.3 million in temporary additional funding to support additional costs and workforce supply pressures resulting from COVID-19 for Residential Aged Care delivered through ACFI subsidies. The temporary funding was in effect from March 1st 2020 – 31st August 2020
- $26.9 million allocated for a temporary 30% increase to the Residential and Home Care Viability Supplements and the Homeless Supplement from March 1st – 31st August 2020.
An additional funding package of $205M was announced on the 1st May saw a one-off payment to Aged Care facilities aiming to support facilities with the additional costs incurred as a result of dealing with COVID-19. For Metropolitan Aged Care facilities the one-off payment was $900 per resident; and $1,350 per resident to for regional facilities.
On the 21 August, the Government announced an additional $170M in funding for COVID-19 related costs. The funding will be injected into pre-existing Aged Care responses and preparedness measures:
- $9.1M for the Victorian Aged Care Response Centre (VACRC) operations
- $89.4M to support the workforce, including additional surge workforce, increased worker training and quarantine costs for interstate workers
- $12.5M to support Residents and their families with grief and trauma support services, for those who have experienced a COVID-19 outbreak
- $9M to the ACQSC to support more quality and compliance checks
- $50.6M for the second instalment of the Aged Care retention bonus
This was followed by an announcement on 31st August – the last day of the Aged Care COVID-19 temporary funding supplement being paid to Providers – of an additional $563.3M to extend the support.
A COVID-19 Support Payment of $245M for all facilities will be paid via Services Australia by early October 2020. This payment is to be used for funding and supporting greater infection control capabilities, staffing costs and communications with families. Reporting on how the funding is used will be required in end of financial year returns. Providers will receive:
- $975 per Resident in major metropolitan areas
- $1,435 (approx.) per Resident in all other areas
The 30% increase to both the Viability and Residential Aged Care Homeless supplements will continue for an additional 6 months (until February 2021).
A third Aged Care workforce retention bonus of $154.5M will also be provided, based on employment as at 30 November 2020.
$71.4M will be provided for the Commonwealth Home Support Program (CHSP), for older Australians who have temporarily relocated from Aged Care facilities to live with family during the pandemic.
An additional $92.4M will also be injected into the Support for Aged Care Workers in COVID-19 (SACWIC) grant, extending the initial period from 8 weeks to 12. You can read more about this grant below.
COVID-19 GRANT OPPORTUNITIES
Grant opportunities for COVID-19 related costs are also available to assist Providers.
- The COVID-19 Aged Care Support Programwill reimburse eligible aged care providers for eligible expenditure incurred on managing direct impacts of COVID-19, opening in March 2020, is taking applications until May 2021. This grant is to reimburse eligible Aged Care Providers for qualified outlays incurred directly as a result of managing COVID-19 impacts.
- The Support for Aged Care Workers in COVID-19(SACWIC) grant is designed to assist approved Providers for workforce costs associated with reducing infection transmission. The SACWIC grant period has been extended to 30 November 2020 with Providers able to apply for funding up until 30 June 2021.
- The targeted Aged Care Business Improvement Fund(BIF) grants announced in January 2020 are available to small to medium sized Aged Care Providers to support improving business operations, transfer ownership to another Provider, or to help deal with the costs of closing down, focusing in particular on those Providers who are in rural and remote regions affected by the 2019-20 Australian bushfires. Applications were set to close in May 2020, however with the onset of the COVID-19 pandemic, grants for the fund have been extended until 30 April 2021. The October budget announcements saw an additional $35.6M in funding for the BIF.
You can read more about the grants here, or if you are eligible for the Business Improvement Fund, or would like to find out more about business improvement strategies throughout the current climate, please call us on 1300 419 119 or email team@providerassist.com.au. We currently have complimentary half hour business strategy review sessions available and would be happy to assist in any way that we may be able.
HOME CARE
A busy period for Home Care news with the budget announcement of 23,000 Home Care packages to be made available immediately. Additionally, the timing for the first phase of the transition to Home Care payments to be made in arrears was released with the budget announcement – with Phase 1 beginning February 2021. The changes intend to bring Home Care in line with other Government-Funded programs, with totals paid in arrears for services delivered. In September, reports alleged that some Home Care Providers had on-charged costs for PPE to care recipients, which was referred to the Aged Care Quality and Safety Commission for investigation.
At LASA’s October Ten Days of Congress event, StewartBrown’s Grant Corderoy presented data showing that Level 4 Home Care Package recipients receive half the hours of care that they would have received 10 years ago. A Home Care Provider disagreed that this was the case, with over-assessment (care-recipients assessed as needing higher levels of care and services than required); funds spent on goods as opposed to services; and the impact of COVID-19 all factors in why care hours are trending down.
Throughout COVID-19, the Commonwealth Home Support Program (CHSP) has eased its referral processes to its services to ensure older Australians could access emergency CHSP services when needed. This allowed CHSP services to be accessed by older Australians for up to 8 weeks without an assessment. This arrangement has been extended from 31 October 2020 to 30 June 2021.
PEAK BODY CAMPAIGNS
Peak bodies LASA, ACSA, the Aged Care Guild, BaptistCare and Anglicare have joined to work together on a campaign intending to lobby politicians and raise community awareness. Working with Apollo Communications, a reputation management firm led by John Howard’s former Media Advisor when he was Prime Minister, LASA CEO Sean Rooney spoke about the campaign at the LASA 10 Days of Congress virtual event. With the impact of COVID-19 on Aged Care, and the media surrounding the crisis, the campaign will aim to educate community perceptions towards Aged Care services, as well as petitioning the Government in the lead up to the May budget.
More work by advocacy bodies with COTA Australia, Carers Australia, Dementia Australia, the Federation of Ethnic Communities Council of Australia (FECCA), the National Seniors Australia and the Older Persons Advocacy Network (OPAN) unifying to release 10 key principles for Aged Care. Prior to the release of the delayed budget in October, the six advocacy groups shared the 10 principles to ensure that older Australians are easily able to access the care and support they need and choose, delivered by a trained and qualified workforce, with a regulator in place to protect consumers and an adequate funding model that can grow with the population as some of the requirements. The first principle also calls for the rewriting of the Aged Care Act; which was also suggested as a future move by Aged Care Minister Colbeck in October, and was a proposed recommendation of the Aged Care Royal Commission’s Counsel Assisting in the Final Hearing.
UNION CAMPAIGNS TARGETING STAFF RATIOS AND TRANSPARENCY
Unions representing Aged Care workers also launched a campaign in September that highlights minimum staffing levels, training requirements and transparency on funding spend. The Australian Council of Trade Unions along with the Health Services Union (HSU), the Australian Nursing and Midwifery Federation (ANMF) and the United Workers Union have developed a four-step plan calling for changes in the Aged Care system which they say has been let down by the Government and critical issues ignored.
Read the media statement with the 4 changes deemed essential here.
The ANMF has also joined forces with the Australian Medical Association, writing to the Government to call for additional measures to be implemented, including more transparency and staff-to-Resident ratios, to prevent COVID-19 outbreaks in Aged Care. You can read the letter written to Prime Minister Scott Morrison here.
AGED CARE QUALITY SAFETY COMMISSION
The Aged Care Quality & Safety Commission (ACQSC) has come under a great deal of scrutiny during the second wave of the pandemic in Victoria and the Royal Commission’s hearings. COVID-19 infection control checks at Residential Aged Care Facilities were to be implemented by the ACQSC across Australia from August. However, a report in mid-October stated that at that stage only two-thirds of the checks had been completed, with over half of Victorian Facilities remaining unchecked. The numbers of unchecked Facilities came under fire and raised the question of whether ACQSC is adequately resourced and funded. This news also came at the same time the ABC reported that ACQSC had spent close to $30,000 on legal advice for Freedom of Information requests by the ABC; and followed previous reports that the ACQSC was too late in enforcing infection prevention standards at Aged Care Facilities that experienced COVID-19 outbreaks. The Aged Care regulator has been described as ‘toothless’ by a staff member.
The ACQSC has released statements on their regulatory activities; and a Provider newsletter for the September / October period, highlighting Provider responsibilities for infection control and feedback on current practices.
VICTORIAN NEWS
The state that has been most gripped by a COVID-19 outbreak in Australia is celebrating a tremendous effort and easing of lockdown restrictions. The Victorian Aged Care Response Centre (VACRC), set up to join both Commonwealth and State Governments to manage the impact of the pandemic in Aged Care, moved in late September to a ‘prevention and recovery’ focus with active cases dropping dramatically. Joe Buffone announced his departure as chief of the VACRC in September (in order to lead the country’s preparation efforts for bushfire season) and was replaced by infectious diseases expert Professor Frank Bowden. You can stay up to date with the VACRC daily operational updates here. A former senior Doctor at the VACRC, Associate Professor Michael Murray, has warned that there is no clear plan for management of another outbreak, with more work needed to be done. The four metro hospital hubs that were to manage Aged Care clusters had also not yet received funding in early October, and there was no clarity on staffing, training and expectations of the hubs.
On the 22 September 2020, the Victorian Government announced $30M in funding to improve Victoria’s public Residential Aged Care facilities. A letter was sent to all Victorian Aged Care Providers, including private and not-for-profit operators, that funding to assist with limiting staff to a single site was to be extended until the end of February 2021. However, unfortunately the contents of the letter only applied to publicly-run Aged Care facilities, and private and not-for-profit operators were emailed to be advised that the funding would not apply to them.
In other Victorian news, there will be ongoing COVID-19 testing of asymptomatic Aged Care workers, once a fortnight in metro regions and once a month in regional areas, beginning 19 October 2020. An additional 7 million P2/N95 face masks were also announced to be provided for Victoria Aged Care facilities.
EMERGENCY PANDEMIC LEAVE FOR AGED CARE RESIDENTS
The emergency legislation implemented in May 2020 that allows Residents the freedom to move out of Aged Care during a crisis (such as the current COVID-19 pandemic) without being penalised, has been extended for a further nine months to June 2021. Under current legislation, Residents can take leave up to 52 days annually for social non-hospital reasons. However, for any additional leave taken, an Aged Care facility will not be provided a subsidy, and these costs are generally passed on to Residents. With the combined crises of both the Australian bushfires and COVID-19, the new Government legislation covers emergency leave (available in times of natural disaster or health epidemics). This ensures that both Residents and Aged Care Facilities who are affected by such circumstances are not financially disadvantaged. You can refer to the Minister’s announcement here, the Emergency Leave legislation here and a Fact Sheet for Providers here.
WORKFORCE
In workforce news, the Fair Work Commission (FWC) has also extended paid pandemic leave for Aged Care workers, until 29 March 2021. The original ruling by the FWC meant workers in Aged Care could access paid leave for two weeks if they needed to self-isolate due to COVID-19 symptoms or if they had been identified as a close contact.
The Aged Care Workforce Industry Council (ACWIC) has been working towards raising standards and training levels in Aged Care, and have been working on an Aged Care Voluntary Industry Code of Practice, with the intention of ‘[uniting] the whole sector behind seven principles to enhance service and process standards’. The ACWIC has also recently announced the launch of a national workforce database, partnering with BPA Analytics, to give Aged Care industry leaders ‘evidence-based snapshot[s]’ of key issues that are important to Aged Care workers. You can read more updates on the work that the ACWIC are doing here.
A model for a research centre proposed by the Aged Care Workforce Strategy Taskforce in their final report from 2018 will be developed by Flinders University in Adelaide and consultancy firm Wells Advisory. Awarded the tender for the Centre for Aged Care Growth and Translational Research (CGTR), the university and firm will develop the operational model for the $34M Aged Care Research Centre.
In late September, the senate enquiry into the Government’s COVID-19 response heard that the $102M allocated to helping the Aged Care workforce deal with the pandemic had used less than a third of the funding. The Government’s announcement in March of the $102M was to provide education and training to the workforce in infection control and allow for the hiring of additional staff. Questions were raised on the cost of the limited tender arrangements. Overall, the inquiry heard that by late September almost 30,000 shifts had been filled by more than 4,000 workers. Aged Care contracting platform Mable, one of the organisations providing the surge workforce throughout the pandemic, was challenged at the Royal Commission by Counsel Assisting that their model was operating outside the regulatory framework.
DEMENTIA UPDATE
In dementia news, Dementia Australia has translated resources built for helping people living with dementia throughout the COVID-19 pandemic into 38 languages. You can view the help sheets and the languages available here.
A new online tool is being piloted to assist family, friends and carers supporting a person’s dementia journey. My Dementia Companion supports people in finding government services and accessing local services, as well as better understanding dementia and developing care and coping strategies. My Dementia Companion was one of the tech idea winners from Dementia Australia’s Decoding Dementia 2019 Innovation Program.
A specialist dementia home, purpose built for caring for people living with severe dementia, is ready to open as the 10th Unit as a part of the Government’s Specialist Dementia Care Program (SDCP). The VMCH Facility in Melbourne can provide care for eight Residents with very severe symptoms of dementia and was refurbished and architecturally designed, guided by Professor Richard Fleming and the Dementia Enabling Environmental Principles.
Monash University’s Centre for Medicine Use and Safety is developing guidelines around the use of psychotropic medications for people living with dementia in Aged Care. With an aim to support the appropriate use of psychotropic medications and reduce the use of chemical restraints, the project is funded by the Dementia Centre for Research Collaboration and is expected to be completed in April 2021. The use of chemical restraints in Residential Aged Care was identified as one of three areas that required immediate action from the Royal Commission’s Interim Report.
TECH, RESEARCH & INNOVATION
To tech, research and innovation, and as always, despite the year that 2020 has been, it is wonderful to see so many new ideas in the Aged Care innovation space. Let’s jump into a quick look at recent developments.
- A ‘dementia avatar’ has won the Victorian iAward in the Not-For-Profit and Community Solution of the Year The AI avatar, known as Ted, represents a person living with dementia and was developed to support carers in learning how to communicate with people living with it. Developed by Dementia Australia and The Applied Artificial Intelligence Institute (A212), Ted assists in educating carers in a ‘safe and encouraging environment’.
- A new AI robot created at Trinity College Dublin will arrive in Australia for further development, potentially as early as 2021. Stevie the Robot was developed to support people living with dementia with many capabilities from medication reminders to video calls to loved ones, to running bingo, quizzes and storytelling games. Although still in development, the trials are looking to explore what Residents and Aged Care workers could want and need from socially assistive robots like Stevie.
- Still in the AI space, and a system originally designed to monitor the health of COVID-19 patients who were in home isolation is being modified for a Residential Aged Care setting. The remote monitoring system, developed by Deakin University’s Applied Artificial Intelligence Institute, the National Trauma Research Institute and Alfred Health aimed to provide clinical and social support, whilst also keeping people isolated. Associate Research fellow Rena Logothetis stated that ‘the principle of care can be adopted more widely’.
- ASX-listed InteliCare has entered the B2C market with a new remote Aged Care platform. Previously only in the Retirement Home and Home Care Provider space, the platform has now opened up as a subscription based service for people living at home. InteliCare uses smart home sensors to gather data on activity in the home and alerts a care team if the sensors detect changes from a normal routine.
- To dementia research, and an interesting new study has found that people with Type 2 diabetes are 5 times more likely to develop dementia; however, the use of the diabetes drug Metformin, the risk rate returns to normal. In a study completed by the Garvan Institute, and UNSW Centre for Healthy Brain Ageing (CHeBA) researcher Professor Katherine Samaras, the link was discovered, although the reason why is as of yet unclear. Researchers are interested in trialling Metformin on people who do not have diabetes.
- Community-centred design and the latest dementia research are the basis for a new Aged Care Facility to be built in South Australia by Clayton Church Homes. Based on a house-type community design, with smaller homes connected by integrated care and hotel services, the community will cater for older people who are no longer able to care for themselves at home. Read more about the features of the design here.
- A sensory blanket for Aged Care Residents living with dementia is being used by Aged Care Organisation Bethanie in partnership with youth-run not-for-profit Sensed. Sensory activities are important for people living with dementia to connect with their memories. The blankets, which have varied textures, sensations, colours and interactive elements have been an important and well-received sensory play option.
Aged Care Accountants Bentleys’ second year of their incubator program CareFactor is currently calling for Providers to pitch their solutions. You can read more here.
ELDER ABUSE
On International Day of Older Persons, 1 October 2020, the Australian Human Rights Commission launched an elder abuse awareness campaign asking people to ‘open your eyes to elder abuse’. With the concern that COVID-19 enhances the risk of elder abuse, the Commission has released a video in which older people share their experiences of elder abuse. You can view the video here.
October also saw the announcement of the removal of a “disincentive for older people to put in place formal ‘family agreements’”. Formal family agreements, also known as ‘assets for care’ arrangements, provides legal protection for the financial rights of older people – with financial abuse considered the most prevalent form of elder abuse.
INTERNATIONAL DAY OF OLDER PERSONS & CARERS WEEK
It is always wonderful to both celebrate and raise awareness on those days and weeks dedicated to the amazing people in our industry. October saw the celebration of both International Day of Older Persons (IDOP) on October 1, and Carers Week, that took place from 11-17 October.
Of course, 2020 has been a very different year to many, and this year’s IDOP reflected the current times with the theme of the year ‘Pandemics: Do They Change How We Address Age and Ageing?’. The theme aimed to highlight the higher risks faced by older persons in pandemics, raising awareness of their special needs and recognising both the roles and contributions older people have in responding. This year is also particularly significant; it is the 30th anniversary of the commemoration, and the first year of the Decade of Healthy Ageing (2020-2030), bringing together experts and society to undertake the Global Strategy and Action plan on Ageing and Health. To find out more information on IDOP 2020, we recommend visiting the IDOP page and particularly checking out this excellent video on changing the way we think about age.
The National Carers Week theme was ‘Tell Us Why You Care’. Run by Carers Australia, the week is focused on brining awareness to people who provide unpaid care and support to family or friends, including those that may be frail or aged. You can find out more about Carers week by visiting their website here.
GOOD NEWS
As always there are still amazing stories of people being simply wonderful humans during this very trying year, and we love reading them. These past months, we stumbled across a great read on 3 older people who are challenging ageing stereotypes by pursuing normal life achievements, health, study and work, despite any age. And once again Captain Sir Tom Moore, the man who walked laps of his garden leading up to his 100th birthday to raise money for charity (approximately $60M AUD was raised), is doing amazing things. Now hosting a podcast series, which aims to help combat loneliness in older people, Captain Sir Tom Moore is encouraging people to ‘donate your words’. The UK’s oldest podcaster, working with charity Age UK and Cadbury chocolate wishes to inspire people to have meaningful conversations with older people. With older people running the risk of being more isolated as a result of COVID-19, the podcast also intends to raise awareness. Titled ‘The Originals’, the interview-format podcast has Captain Tom interviewing older people about their lives and life advice and can be found to listen to on Spotify here. An exceptional listen!
 |
LISSIE LYONS – CHAMPION OF EDUCATION & MARKETING Author |




